The Accreditation Digest is a newsletter to help keep you informed and educated throughout our Accreditation process, as we prepare for our Accreditation visit.
The Accreditation Digest is a newsletter to help keep you informed and educated throughout our Accreditation process, as we prepare for our Accreditation visit.
A Guide to Required Organizational Practices (ROPs)
Required Organizational Practices (ROPs) are a very important part of our Accreditation. If any of these practices are not in place, we cannot achieve Accreditation. For this reason, it’s very important that all of our teams are aware of the ROPs and know where to find information about them. See the 16 ROPs below with a brief summary on what these standards are, and how we’re meeting them.
1. The governing body demonstrates accountability for the quality of care provided by our organization.
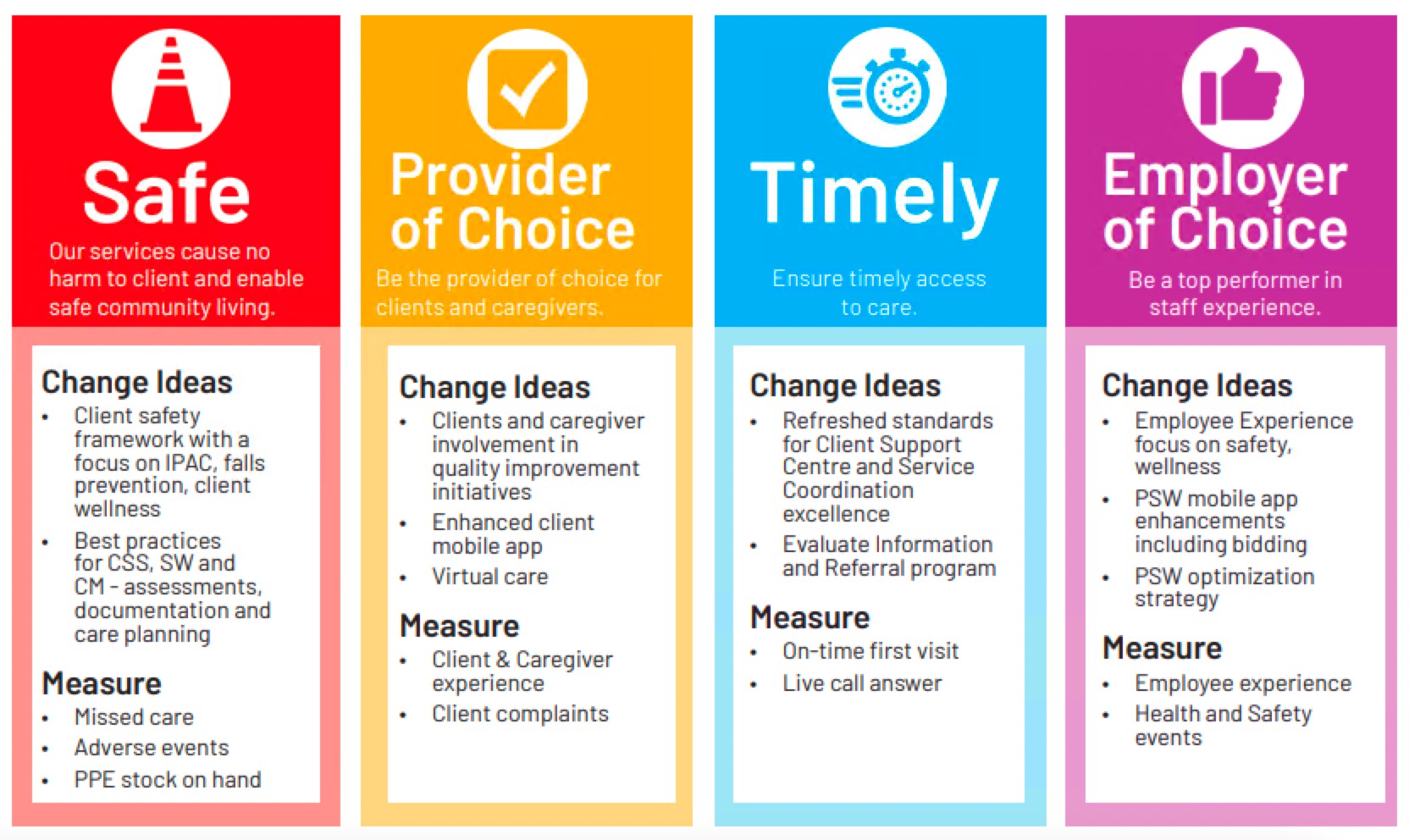
The Quality Subcommittee of the Board meets regularly to review quality metrics and performance. The Quality Improvement Plan is aligned with Strategic Planning and approved by the CEO and the Senior Operations Team.
2. A documented and coordinated approach to prevent workplace violence is implemented.
Our Workplace Violence Policy outlines processes in place to prevent and address workplace violence. The Joint Health & Safety Committee reviews workplace violence and risks on a quarterly basis and provides recommendations for action.
3. A preventative maintenance program for medical devices, medical equipment, and medical technology is implemented.

We are in the process of standardizing our approach to preventative maintenance, watch for an upcoming Accreditation Digest outlining the plan.
4. Patient safety training and education that addresses specific patient safety focus areas are provided at least annually to leaders, team members, and volunteers.
Training is provided to all staff on hiring through Dayforce. Volunteers receive training on Client Safety through their orientation manual. All staff and volunteers receive regular education through newsletters and other communications. Yearly attestations are completed with staff. .

5. A patient safety plan is developed and implemented for the organization.
The 2022 Client Safety Plan identifies our key priorities for client safety and the strategies underway.
6. A patient safety incident management system that supports reporting and learning is implemented.
Key word flagging reports from EasyCare are used to compile incident data which is reviewed on a weekly basis. Metrics regarding incidents are shared monthly through the heat map. Clients receive information on how to report concerns or complaints in the welcome package. The policies on Client Safety Reporting and Event Reporting outline our response to safety incidents.
7. A documented and coordinated approach to disclosing patient safety incidents to clients and families, that promotes communication and a supportive response is implemented.
Our Disclosure of an Adverse Event policy outlines our response to risk and safety events. When high risk or adverse events occur, a debrief takes place where a root cause analysis is conducted and areas of opportunity are identified and addressed.
8. The governing body is provided with quarterly reports on patient safety that include recommended actions arising out of patient safety incident analysis, as well as improvements that were made.
The Director, Quality, Risk and Performance prepares quarterly reports to share with the Quality Subcommittee of the Board which outline key metrics related to quality and risk and mitigation strategies underway.

9. To minimize injury from falls, a documented and coordinated approach for falls prevention is implemented and evaluated.
The 2022 Falls Prevention Strategy and our policy on Falls Prevention outline our response to falls and strategies in place to prevent falls among our clients.
10. Working in partnership with clients and families, at least two person-specific identifiers are used to confirm that clients receive the service or procedure intended for them.
Our Two-Factor Identifier policy outlines our approach and all staff and volunteers receive training during orientation.
11. Information relevant to the care of the client is communicated effectively during care transitions.
Our policy on Client Transitions covers this.
12. A safety risk assessment is conducted for clients receiving services in their home.
Our policy on Home Safety Inspections covers this, with inspections being completed during initial and follow up assessments.
13. Hand hygiene education is provided to team members and volunteers

All team members and volunteers receive training during orientation. Educational materials are provided annually during the week of World Hand Hygiene Day. A report on hand hygiene is currently being compiled- stay tuned for an upcoming Accreditation Digest.
14. Compliance with accepted hand hygiene practices is measured.
Clients are asked about the hand hygiene practices of our staff during satisfaction surveys and the results are shared with team members yearly during the week of World Hand Hygiene Day.

15. Processes for cleaning, disinfecting, and sterilizing medical devices and equipment are monitored and improvements are made when needed.
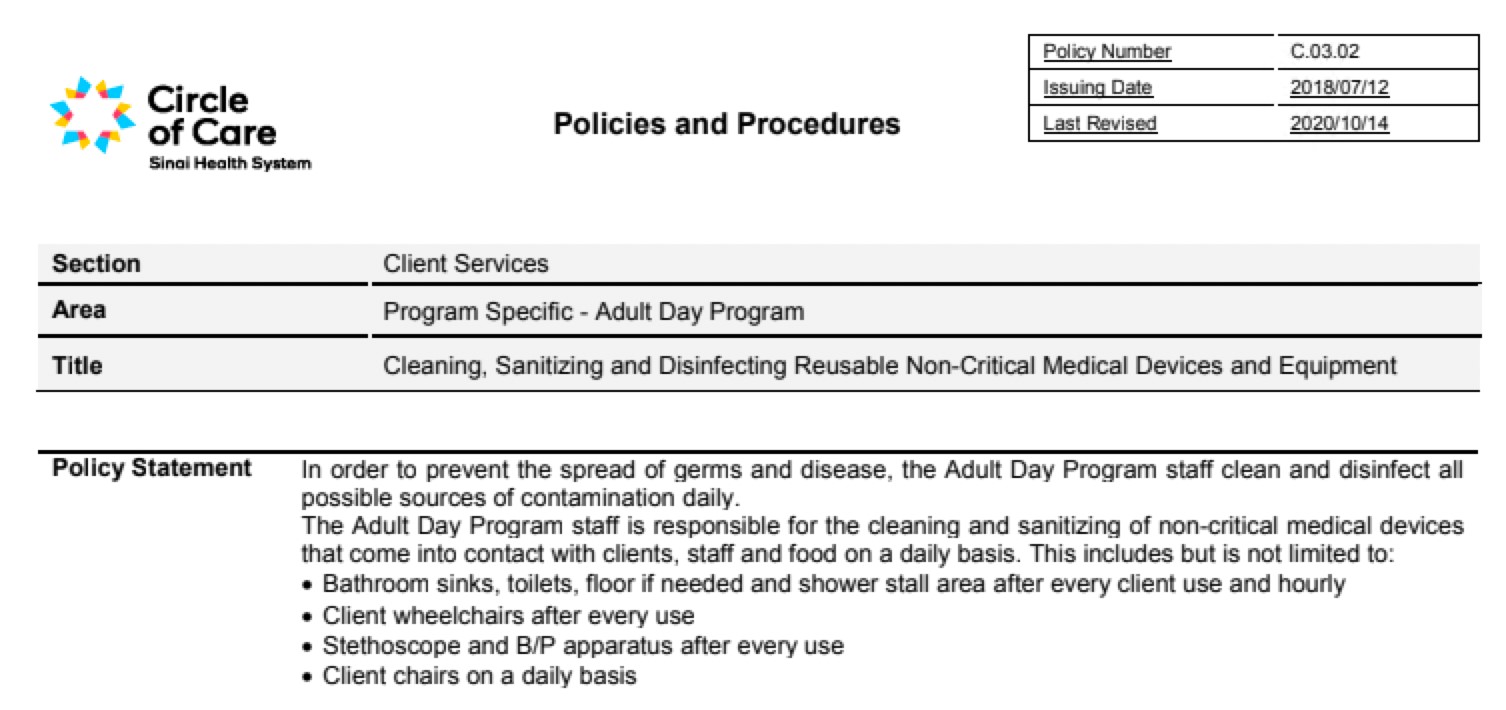
All of our locations have always had cleaning procedures in place. In response to the COVID-19 pandemic, additional measures that align with Public Health recommendations were put in place. Our ADP has the most in-depth procedures, which you can find outlined on the policy on Cleaning, Sanitizing and Disinfecting Reusable Non-Critical Medical Devices and Equipment as well as the policy on Cleaning Surfaces.
16. A documented and coordinated medication reconciliation process is used to communicate complete and accurate information about medications across care transitions.
Medication reconciliation is not conducted internally. Regulated staff include medication management in the client assessment if needed. The regulated staff can encourage the client to connect with their pharmacist to reconcile their medications if needed. Our policy on Medication Management outlines when we can safely delegate medication management to our home service workers. The ADP Medication Management policy outlines the process for supporting with medications for ADP clients. Our policy on High-Alert Medications outlines that high-alert medications are never to be administered or delegated by any Circle of Care staff. If the medication becomes part of routine medications and is in a blister pack, PSWs can remind the client to take the medication, but it must be self-administered.