- Familiarize yourself with the area
- Plan the safest route to and from the client’s home
- Know emergency numbers
- Know the local transit route
- Do not give clients personal phone numbers. Use call block
- Apprise Head Office of location, time and estimated duration of visits
Safety In The Community
Worker Strategies
Pre-Visit Strategies
Travelling in the Community
- Dress conservatively. Wear appropriate footwear.
- Wear light colored clothing for evening visits.
- Use elevator safety tips
- If using public transit sit in designated safety areas. If empty sit close to the driver.
- Stay alert and mindful of surroundings.
- Keep to well lit routes & well traveled streets. Do not take short cuts.
- Walk briskly and with purpose. When possible keep hands free.
- Walk against flow of traffic. Never wear headphones or text messaging while walking.
- Do not walk through a crowd or engage in conversation with strangers
- Avoid using public phones and ATM machines in unfamiliar areas
- If someone tries to rob you give up your property
- If you are being followed in your car drive to the nearest ‘safe’ building
- If you think you are being followed walking, cross the street, walk to the nearest open store or restaurant
- Never allow someone to force you into a vehicle. Fight back. Roll under your vehicle if possible.
Car Safety Tips
- If you are being followed in your car drive to the nearest ‘safe’ building
- If you think you are being followed walking, cross the street, walk to the nearest open store or restaurant
- Never allow someone to force you into a vehicle. Fight back. Roll under your vehicle if possible.
Some suggested items to keep in your vehicle:
- Booster cables
- cloth or paper towels
- compass
- emergency food pack
- extra clothing
- fire extinguisher
- ice scraper and brush
- survival candle and matches
- sand, salt or kitty litter
- shovel, tow chain
- flares
- traction mats
- Flashlight
- First Aid survival kit
- Survival blanket
- A Call Police Sign
Client Home Visits
- Never enter a home not scheduled for a visit.
- Exercise care in hallways, elevators and
stairwells. - Stick to the centre of the hallway. In an emergency, knock on as many doors as possible and yell “FIRE”.
- Do not enter a home if there is a visible threat to your safety.
- When entering a home, PAUSE and assess the situation. Locate the phone, any obstacles to exits.
- Introduce yourself, state the purpose of your visit. Wait to be invited in.
- Avoid being “trapped”.
- Leave your shoes on or bring appropriate footwear.
- Do not bring valuables into the clients home.
- Always leave an exit route.
- Avoid interviews in the kitchen
- Recognize the first signs of change in your client’s behaviour or others in the home.
- Leave if you are asked to leave
- Immediately report unusual occurrences
- Attend training on how to recognize and diffuse aggressive behavior.
Protection Against Client Agression
General Risk Factors of Client Aggression:
Client’s Physiological Conditions:
- Systemic disorders:
- fluid/electrolyte imbalance, anemia, thyroid disorders, diabetes, hepatic disorders, neurological disorders, epilepsy, degenerative diseases
- Toxic levels of medications
- Psychiatric Conditions:
- psychotic symptoms & paranoia, psychogeriatric illness
- Substance abusers
Approaches to Aggression Prevention
- Focus on methods to manage, contain or reduce the impact of the aggressive act
- Be mindful of body language
- Observe the client’s movements
- Avoid arguing
- Ask open ended questions
- Acknowledge the client’s answer(s)
De-escalation techniques:
- Observe the client’s movements
- Try to appear calm, self-controlled and coherent
- Ensure non-verbal communication is non-threatening
- Engage in conversations acknowledging feelings and concerns
Dementia – Considerations for Care
- Behaviour is a form of communication
- Search for the meaning behind the message and incorporate that into your care
- Concentrate on the person, not the task
- Aggressive behaviour can be a “responsive behaviour”
Dementia
- Results in the loss of ability to think clearly and act purposefully
- Loss of self awareness, memory, language and purposeful movement
- May have altered perception, low attention span, or apathy
Client Self-Protection signs:
- Pacing
- Restlessness
- Sarcasm
- Swearing
- Increased loudness
- Rigid posture
- Gripping
- Clenched fists
Communication strategies:
- Use the person’s name
- Make eye contact
- Speak slowly and clearly
- Connect with the past
- Validate their feelings
Responding to Challenging Behaviours
- Be aware of triggers
- Ask what is wrong
- Look for favourite activities & traditions
- Use positive verbal & body language
- Ask him/her to stop gently
- Ask others for success stories
General Risk Factors and Hazards
Assessing Unsafe Conditions in the Home Environment
- Exterior/entrance to the building/home
- Chemical/biological/environment hazards
- Fire hazards
- Physical/ergonomic hazards
- Fall hazards
- Personal safety hazards
Exterior/Interior of Home:
- Obstacles
- Building not safe
- Clutter
- Poorly illuminated
- Lack of handrails
- Ice/snow
- Aggressive animals
- Pests
- Cigarette smoke
- Gasoline, solvents, paints improperly stored
- Compressed gas
- Improperly located smoke detectors or no smoke detectors
- Lack of portable fire extinguishers
- Lack of parking/safe
parking - Home located in high risk area
- People “hanging” in area
- Lack of building security
- Exits lacking/blocked
- Presence of drugs or weapons
- Inadequate heat/ventilation
- Unsafe/inadequate or faulty equipment
- General unsanitary conditions
Your Safety is a Priority
Learn about potential risks in the community and practical tips and strategies for navigating these risks.
Safe Driving
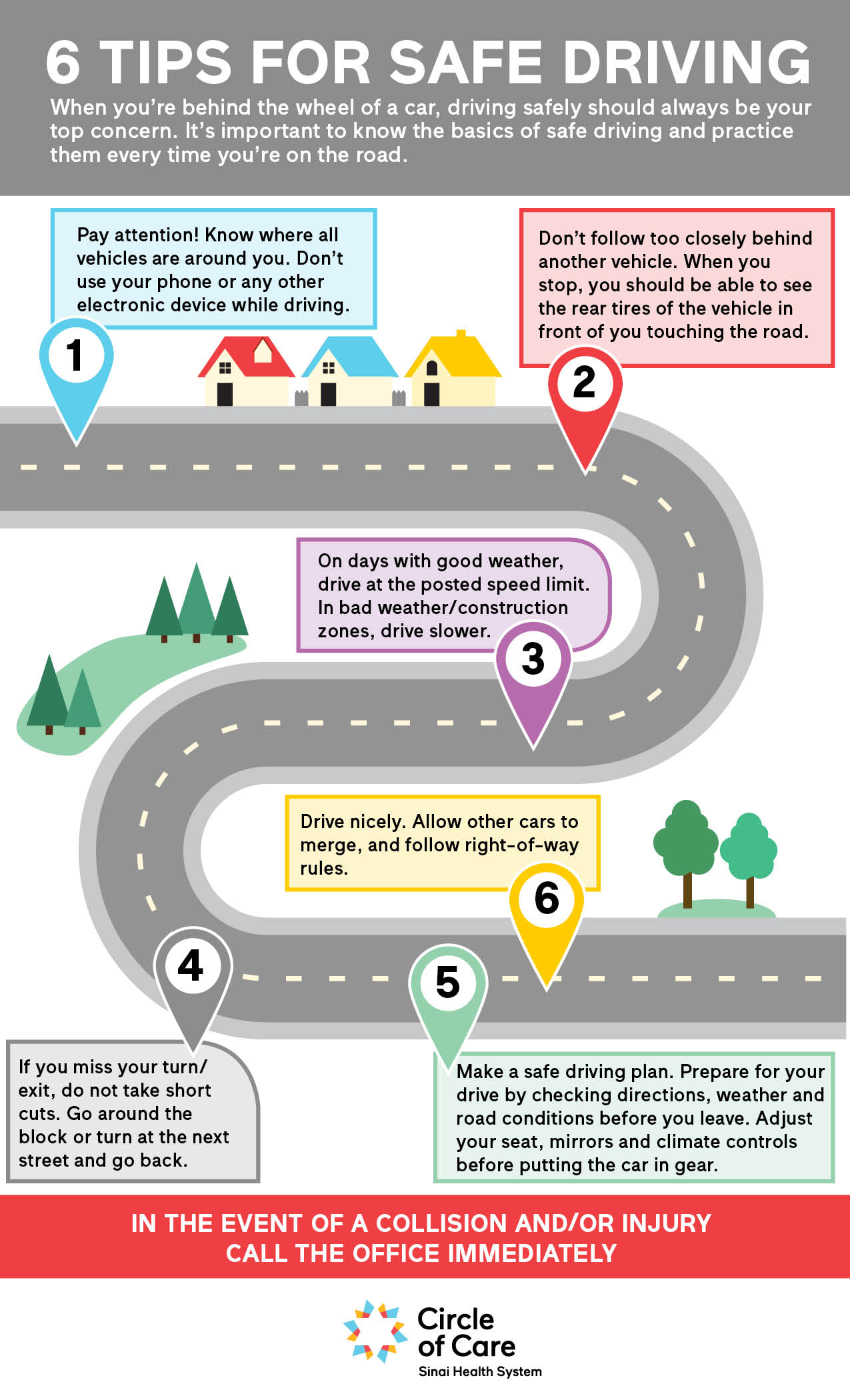
- Pay attention! Know where all vehicles are around you. Don’t use your phone or any other electronic device while driving
- Don’t follow too closely behind another vehicle. When you stop, you should be able to see the rear tires of the vehicle in front of you touching the road.
- on days with good weather, drive at the posted speed limit. In bad weather/construction zones, drive slower.
- If you miss your turn/exit, do not take shortcuts. Go around the block or turn at the next street and go back.
- Make a safe driving plan. Prepare for your drive by checking directions, weather and road conditions before you leave. Adjust your seat, mirrors and climate controls before putting the car in gear.
- Drive nicely. Allow other cars to merge, and follow right-of-way rules.
Preventing Workplace Violence

- Circle of Care is committed to the prevention of workplace violence and to a violence-free workplace.
- Any act of violence committed by or against anyone is unacceptable conduct that will not be tolerated. Every effort has been made to identify possible sources of violence and to implement procedures to control the risks.
- No employee, volunteer, or any other individual associated with Circle of Care shall subject any other person to workplace violence or allow or create situations that allow workplace violence to occur. Everyone is expected to uphold this policy and to work together to prevent workplace violence.
To review our policy on Workplace violence, click the button below.
Taking Care of Yourself
- Wear comfortable and appropriate clothes and shoes to work
- Be sure to eat regularly (don’t come to work without eating breakfast; take a lunch break), exercise regularly (if you don’t follow an exercise routine, you can maintain your health by lots of walking!) and get plenty of sleep
- If you are ill or contagious, don’t go to work. As well as taking care of yourself you must protect your clients who might be elderly people, susceptible to infection
- If you know that your client has a communicable disease be sure to report this to your supervisor
- If you smoke, try to quit or cut down
- Be aware of the dangers of excessive use of alcohol and non-prescription drugs
- Let your coordinator know if you are stressed out or feeling down. Sharing problems is a great way to solve them. Keeping things inside often increases your level of stress.
- Taking vacation time will help you to manage stress
Safe Footwear to reduce Slips, Trips and Hazards

- Wear only closed shoes
- Wear shoes with flat or low heals
- Wear shoes with soles that are not slippery
- Sandals, slippers, thongs/flip-flops, and high-heeled shoes are not to be worn on the job as they could cause you injury
- Never work in bare or stocking feet
Safe Operating Procedures
Safe Driving
|
Circle of Care
|
Driving Safe Operating Practice |
SOP # |
|
Revised:
|
||
| Training and Competency |
|
|
| Hazard(s) |
|
|
| Injury Potential |
|
|
| Energy Source(s) | · Gasoline/propane/electricity | |
| Applicability | · All staff who drive a vehicle during work | |
| PPE | · Seat belt | |
| Pre-use Checklist |
|
|
| Safety Precautions |
|
|
| In the Event of a Collision and/or Injury |
|
|
| Sequential Steps to Complete the Work Safely |
|
|
| Preventative Maintenance | · Maintain the vehicle as per the manufacturer’s recommendations in the vehicle manual | |
| Comments | ||
Slips, Trips, and Falls Prevention for Workers
| Training and Competency |
· Training on slip, trip and fall hazards · Inclement weather, hazardous walking conditions, bathroom safety |
| Hazard |
· Exposure to slippery or wet floor surfaces or poor winter weather conditions · Surface contaminants on floors that cause loss of traction (snow, water, grease, dirt) · Working in wet areas such as bath/shower rooms · Inappropriate footwear · Inappropriate behaviour such as running to catch a bus, being distracted by being on a mobile phone, rushing, not following established safe work procedures, etc. · Flooring with poor traction or slip resistance such as a wet bathroom floor · Obstructions, obstacles and trip hazards left in high traffic pathways · Rushing to get to a client on time or rushing when clients may be booked too close together not giving enough time to travel or trying to reach the client at the scheduled time, particularly when the weather is poor |
| Injury Potential |
· Bruises and contusions · Strains and sprains · Fractures |
| Energy Source(s) | · None |
| Applicability | · All employees |
| PPE | · Slip resistant soles on shoes |
| Pre-use Checklist | · None |
| Safety Precautions |
· Be aware of surroundings always in client home and office · Take extra care when walking in poor weather & leave early to get to your first client to avoid rushing · Do not rush or run especially when trying to catch a bus · Roll up loose rugs at a client home · Ensure the necessary bathing equipment is available for you to assist the client safely. If no equipment is available or the client refuses to use it, the PSW should do a sponge bath · If client appointments are booked too close together notify your Service Coordinator that you are rushing in inclement weather. Tell the Coordinator the client names & let them know why you are late |
| In the Event of Injury | · Seek medical attention if needed & call your Coordinator or after-hours phone immediately to report the incident |
| Sequential Steps to Complete the Work Safely |
· Ensure loose floor mats do not pose a slip or trip hazard & pick up or remove when providing care. Ask client if you can move them & put them back after · Clean up spills when they happen · Keep walking areas free of clutter, furniture. If client home is cluttered and poses a hazard, contact your Supervisor to help identify corrective actions with client and/or family members · Report all hazards to your supervisor · Avoid running or rushing to get to the next client appointment · Use proper positioning when assisting a client on stairs · Ensure there is safe access to a client’s home. Do not try to walk through dangerous conditions where there is construction or take short cuts |
| Lockout Steps | · None |
| Preventative Maintenance | · Check shoes to ensure that the sole is in good shape and replace when worn. No heels on shoes or no flip flops can be worn at work, only closed toe and heel shoes are to be worn |
| Comments | · Refer to Footwear Policy |
Last Updated: June 21, 2023
Good Body Mechanics
|
Good Body Mechanics Safe Operating Procedures |
SOP # | |
|
Revised: May 2018
|
| Training and Competency | · Awareness of & tips for practicing good body mechanics to reduce the risk of musculoskeletal injuries |
| Hazard |
· Not aware of or using safe body mechanics · Not practicing correct body mechanics, working too quickly or trying to reach away from your body · Risk of MSD injuries when good body mechanics are not used |
| Injury/Illness Potential |
· Strains and sprains from using poor body mechanics
|
| Energy Source(s) | · None |
| Applicability | · All staff |
| PPE | · Sturdy, comfortable shoes with a slip resistant sole |
| Pre-Use Checklist |
· If there is a second caregiver, check that they know what they need to do to assist · If there is assistive devices (lifts, walkers or slings) know how to use them and position them properly so you are ready to use them without reaching or pulling the client |
| Safety Precautions |
· Maintain your physical wellbeing. Stretch, strengthen your abdominal muscles · Ensure you take time to rest between tasks that are repetitive · Get enough sleep (6- 8 hours each night) · Take time to de-stress and relax · Report changes in your client’s condition to your Supervisor · In the event that a transfer requires 2 persons (as per care plan) & a 2nd person is not present, DO NOT attempt to transfer alone · Modify care to ensure your safety · If you are being asked to do something that you feel is not safe, call your Coordinator or the CSS · If the client transfers are difficult or become more hazardous contact the Nurse (CSS) to request that an OT or PT come to assess |
| In the Event of Injury | · Report to your supervisor immediately |
| Sequential Steps to Complete the Work Safely |
· Know each step of the task · Plan ahead to reduce the need to take short cuts · Know your client and their abilities. Ask them to help you wherever possible. Communicate to client exactly what you are doing · Keep you back in the neutral position (bend at the hips and/or knees) · Keep a wide base of support (plant your feet at least shoulder width apart) · Keep people & objects as close to your body as possible (holding heavier objects away from your body takes more effort and puts more stress on the muscles) · Do not twist when carrying, pushing or crouching. Move or change your feet to point them in the direction you are going · Tighten your abdominal muscles when lifting or when starting to push · If you are working with another person, keep up communication so both parties know what to expect · Use a standing kneel lift to reach or assist clients across a bed. Stand close the bed. Place one knee on the side of the bed, tighten the abdominal muscles and reach or assist a client to turn · Reduce the load and divide it into smaller weights whenever possible · Sleep on your back or side as opposed to your stomach · If needed, place a pillow under your knees (for back sleeping) or between your knees if on your side · Keep a neutral head posture, keeping your head directly over your neck with the chin tucked in slightly. Keep the ears over your shoulder
|
| Lockout steps | · None |
| Preventive Maintenance | · None |
| Comments |
[
|

Client Agression
|
Circle of Care
|
Aggressive Behaviour in Clients Safe Operating Practice |
SOP # |
|
Revised:
Date: April 2012 |
| Training and Competency |
· All Personal Support Workers · Fundamental education on cognitive deficits
|
| Hazard(s) |
· Inappropriate behaviour towards caregivers · Unprovoked or sudden actions by resident during care · Resident becomes resistive to care and display responsive behaviours such as biting, spitting, kicking, grabbing, punching, and/or scratching of employee who tries to provide or assist with care · Resident shows verbally abusive behaviour towards staff during care
|
| Injury Potential |
· Bruises, scratches and contusions · Strains and sprains · Fractures
|
| Energy Source(s) |
|
| Applicability |
|
| PPE |
|
| Pre-use Checklist |
· Assess and gauge receptiveness of client prior to approaching to determine temperament and mood at that time · Stand at the front door before entering the room and introduce yourself · Try to find out any established triggers for behaviours · Review the care plan, and assessment history for the client to learn about their preferences, temperament, dislikes, former occupation and hobbies · Take opportunities to speak to family members if possible to learn more about the client’s likes and dislikes |
| Safety Precautions |
· Do not rush or force client · Continually gauge temperament and be aware of changes or early warning signs that may indicate escalating behaviour such as clenched fist(s), silence, changes in facial expression or any other changes from normal behaviour · Understand the unique ways that are specific to each client and assess any changes, stopping or re-directing your behaviour to reduce or eliminate what is triggering the different behaviour
|
| In the Event of Injury |
· Seek medical attention if needed
|
| Sequential Steps to Complete the Work Safely |
· Re-assess each client before each encounter, ask for permission and explain what you would like the client to do · Understand that the client may not recognize you or understand your communication or language and may have forgotten how you fit into their life · When entering a room, introduce yourself, use eye contact and gestures. For example, if you need to assist the client to get up, raise your hands in a gesture. When talking, speak slowly and allow for silences so the resident can process the information · You should know if the client is currently on a tranquilizer or any other medication that has a sedating effect, to help you understand that they may be slower than usual or not as attentive · Break the task into individual steps and explain what you are doing and what will be happening next. Prepare them for the experience so they can prepare for each sensation such as a warm bath or a wet cloth · Offer verbal reassurance when things are going well, using a soft voice and tone. Try not to speak in monotones without any expression · Avoid reacting with adverse facial expressions or words and tone of voice when something goes wrong. This could escalate a situation
|
| Lockout Steps |
|
| Preventative Maintenance |
|
| Comments |
Working Alone
|
Circle of Care
|
Working Alone Safe Operating Practice |
SOP # |
| Created April 2012 Revised: Date: October 2018 |
| Training and Competency | · Working alone presentation |
| Hazard(s) |
· Personal safety concerns and associated injuries · Injury from exposure to unknown hazards because of work in unfamiliar areas/homes |
| Injury Potential |
· Assault, various injuries as a result of aggressive acts · Cuts, bruises, fractures, emotional trauma |
| Energy Source(s) | · None |
| Applicability | · All staff who work in the community alone |
| PPE | · Cell phone |
| Pre-use Checklist |
· Assess the home environment for risks prior to beginning work · For all new client areas analyze the safest route to take/ensure buses run at times you need access · Ensure cell phone is accessible and charged |
| Safety Precautions |
· Familiarize yourself with any new areas · Plan the safest route to and from the client’s home · Know emergency numbers & program them into your phone · Know the local transit route · Do not give clients personal phone numbers. Use call block · Dress conservatively. Wear appropriate footwear. · Wear light colored clothing for evening visits. · Use elevator safety tips. Do not get on the elevator 1st if you are uncomfortable or do not get on if someone is there who you do not feel comfortable with · If using public transit sit in designated safety areas. If empty sit close to the driver. · Stay alert and mindful of surroundings. · Keep to well-lit routes & well-traveled streets. Do not take short cuts. · Walk briskly and with purpose. When possible keep hands free. · Walk against flow of traffic. Never wear headphones or text message while walking · Do not walk through a crowd or engage in conversation with strangers · Avoid using public phones and ATM machines in unfamiliar areas · If someone tries to rob you give up your property · If you are being followed in your car drive to the nearest ‘safe’ building · If you think you are being followed walking, cross the street, walk to the nearest open store or restaurant · Never allow someone to force you into a vehicle. Fight back. Roll under your vehicle if possible. · Keep vehicle in good running order · Check your car before getting in · Have your keys in hand · Know where to park your vehicle. Park in well-lit areas. · Never enter a home not scheduled for a visit. · Exercise care in hallways, elevators and · Stick to the center of the hallway in an apartment building. In an emergency, knock on as many doors as possible and yell “FIRE”. · Do not enter a home if there is a visible threat to your safety |
| In the Event of Injury |
· If you are in immediate danger, call 911 · Notify your supervisor immediately · If you seek medical attention notify your supervisor |
| Sequential Steps to Complete the Work Safely | · See safety precautions as each situation will require different steps |
| Lockout Steps | · None |
| Preventative Maintenance | · Ensure all proper preventive maintenance is maintained for all vehicles used for work |
| Comments |
Biological Hazards Exposure
|
Circle of Care
|
Biological Hazards Exposure Safe Operating Practice |
SOP # |
|
Revised: New
|
|
Training and Competency |
· Infection Prevention and Control Practices |
| Hazard(s) |
· Exposure to potentially infectious organisms · Exposure to unknown potentially infectious products, materials, surfaces and blood and body fluids |
| Injury Potential |
· Occupational illnesses and disease · Risk of cross contamination exposing employees and clients to illness causing organisms |
| Energy Source(s) | · None |
| Applicability | · All employees |
| PPE |
· Non-latex, no powder disposable gloves · Fluid resistant face masks (when there is a risk of spraying or splashing into the face) · N95 fitted respirator (when there is exposure to airborne pathogens) · Fluid resistant gown (where there is a risk of spraying or splashing potentially infectious microorganisms onto clothing & only as instructed by Circle of Care) · Safety glasses (if there is a risk of spraying or splashing of infectious microorganisms where client is sick with frequent coughing, sneezing) |
| Pre-use Checklist |
· All PPE for biological hazards except safety glasses are one time use only and are to be disposed of immediately after use · Safety glasses are to be disinfected using hand sanitizer or alcohol wipe) |
| Safety Precautions |
· Do not wear an N95 unless it has been fit tested and approved for use · Ensure all PPE is kept in a clean dry area protected from dust and humidity |
| In the Event of an Injury |
· Seek medical attention if needed · Notify supervisor |
| Sequential Steps to Complete the Work Safely |
· COC willcommunicate information on clients where enhanced precautions necessary · Read the care plan or contact your CSS if you have any concerns Use routine precautions (wash hands before & after contact) for all persons and before preparing, handling or serving food, after servicing or cleaning potentially contaminated equipment or materials, when handling soiled linen, after personal body functions (using the toilet, blowing your nose, smoking, etc.) · Use proper hand washing sequence and wash hands for 10 – 15 seconds · Verify what if any PPE are required prior to performing personal care · Use an alcohol-based hand sanitizer as an added precaution during outbreaks or when caring for a person who has a communicable illness · Keep nails short and clean · Follow the policy on staying home if you are sick with frequent coughing, fever or diarrhea · Report all concerns of potential infections to your Coordinator or CSS · Get vaccinated to protect yourself and those you care for |
| Lockout Steps | · None |
| Preventative Maintenance | · Ensure safety glasses are maintained in good repair and disinfected before and after use |
The Rights of The Worker
The Right To Know
- Job-related hazards
- Safety Hazards
- Health Hazards
- Latency period
- How the hazard can harm them
- How to control the hazards
The Right To Participate
- As a member of the Joint Health and Safety Committee or Health and Safety representative
- To make accommodation about health and safety in the workplace
- Asking questions and being consulted
The Right To Refuse Unsafe Work
- Can refuse work that puts themselves or another worker at risk. There is a defined procedure to do this:
- Must tell employer
- Employer must investigate
Bed Bugs
Circle of Care works hard to provide our staff with the safest work environment possible. If we are notified that a client’s home has a bed bug infestation you will be notified immediately and advised on how to protect yourself, your clients, and your family/home. It is important to respond promptly and sympathetically to clients and family members who report bed bug problems to you directly, or if you suspect that a client may have an infestation. In such a case, please call into the office to report immediately to a live person so that a note can be made on the client’s file, and that your supervisor and any other necessary individuals can be notified for a greater chance of quick control.
Please use the following as a reference for monitoring the signs of a possible bed bug infestation, and how to protect yourself:
- What are the signs of a bed bug infestation?
- Blood stains, spots, streaks from crushed bugs on bed sheets.
- Rusty or tiny black spots of excrement on sheets, mattresses, bed clothes, walls
- Eggs – when ready to hatch they are the size of a grain of rice.
- Egg shells/shedded skins
- An offensive sweet musty door when infestations are severe.
- Bites on skin – usually in a cluster or linear pattern
- Pets scratching bites
- Where do we find bed bugs?
- Beds – in tufts, seams and folds of mattresses, cracked bed frames.
- Wall hangings, drapery pleats, behind mirrors
- Any narrow space or crevice- window/ door frames, baseboards, cracks in walls, floor cracks, cracked furniture
- Under/inside wallpaper, electrical boxes, etc.
- Who is at risk of getting bed bugs
- Residents in multi-unit dwellings (apartments, retirement homes, condos, etc.)
- Individuals living in group situations (group homes, shelters, etc.)
- Ultimately, anyone can get them.
- Before going into a client’s home:
- Wear old clothes if possible
- Avoid wearing pants with cuffs, tuck pants into socks
- It is recommended that you wear tight fitting clothing or tie clothing clothing close to the body.
- Light coloured clothing is also better to see any bugs that may on your clothing.
- While in a clients home:
- Avoid sitting on furniture (if needed, sit on a hard surface without fabric)
- Meet in a setting where bed bugs are less likely to be present (kitchen area). If possible try to avoid the bedroom or sleeping areas
- Limit the number of personal items you are bringing into the home. Leave them in the car or put them in a plastic bag
- Hang your bag or coat on a door knob or hook instead of on the floor or a chair.
- Leaving a client’s home:
- At the door or outside of the home, inspect your clothing and personal belongings and stamp your feet firmly ( as if knocking snow/mud off of your boots)
- If possible keep a change of clothes available and place the work clothing in a plastic bag or container.
- Once you are at home:
- Remove outer clothing immediately, keep separate from general laundry
- If time permits, put in HOT dryer for 20 minutes
- If no time, put clothes in a garbage bag and tie it until it can be laundered or put in a hot dryer for 20 minutes.
- It is recommended that employer:
- Schedule the visit at the end of the workday.